In the era of precision medicine and molecular oncology, persons with cancer are gaining access to increasingly advanced forms of treatment. However, while some may be able to benefit from this cutting-edge clinical innovation, many underserved patients are still struggling to receive care. A new law in Massachusetts is set to eliminate a major financial barrier to accessing clinical trials. Lawmakers, health care practitioners, and other stakeholders behind the measure hope that the provision contained in the health care bill “promoting a resilient health care system that puts patients first” will increase access to care for all, regardless of their sex, age, race, ethnicity, or socioeconomic status.
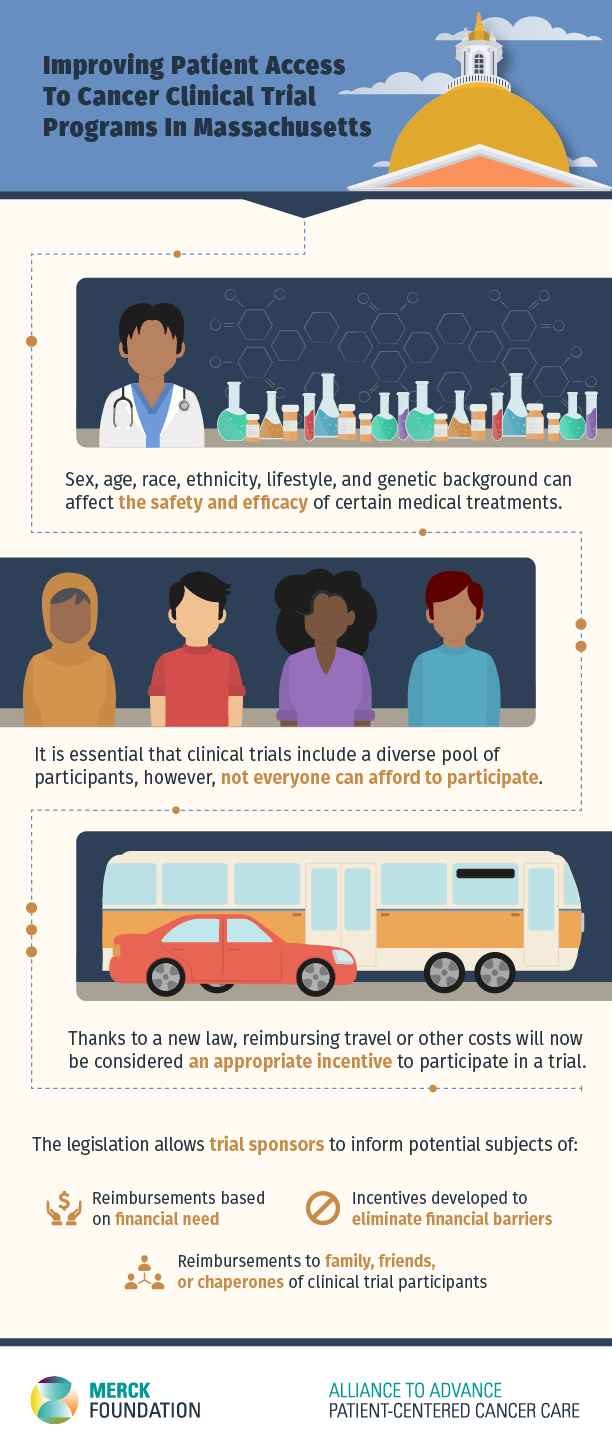
While it is an established fact that sex, age, race, ethnicity, lifestyle, and genetic background can affect the safety and efficacy of medical treatments, clinical trial populations often do not reflect the diversity and heterogeneity of our society. According to articles and commentaries published by JAMA Oncology and Nature, a majority of clinical trials either fail to capture crucial demographic data or neglect to include a representative sample of Black, Indigenous and People of Color (BIPOC) participants. Out of the 230 clinical trials analyzed in one study, only 63% included any information about the race and ethnicity of study participants. When this type of demographic data was included, it painted a grim picture of recruitment trends. African American and Hispanic/Latino patients were consistently underrepresented, with data even showing a slight reduction in recruitment of African Americans through the years.
Beverly Moy, MD, MPH is the Clinical Director of the Breast Oncology Program, Director of Community Outreach, and a medical oncologist at the Massachusetts General Hospital Cancer Center. She is also one of the clinical investigators with the Alliance to Advance Patient-Centered Cancer Care and a member of the advisory council for the Lazarex Foundation. Dr. Moy worked with the Foundation to develop a clinical trial bill that expands access to care in Massachusetts. From her perspective, access to clinical trials and social justice are closely intertwined: “Access to cancer clinical trials is an important health equity issue. In this era of molecularly-driven precision medicine, sometimes the best treatment option for a patient with cancer is a clinical trial. If patients lack access to clinical trials, they are being deprived of some of the best treatment options. I feel strongly that this is a social justice issue.” There are many reasons why Black, Indigenous and People of Color (BIPOC) may not be participating in clinical trials at the same rate as their white counterparts. Some may feel mistrust towards the medical establishment, potentially due to a well-documented history of racism and discrimination. For others, particularly those of lower socioeconomic status, there may be other barriers.

As Dr. Moy explains, while most cancer therapies usually require regular visits to the hospital, participating in a trial requires an even more extensive time commitment. Trial participants need to rely on personal resources to participate: “there’re just a lot more appointments when you enter a clinical trial. And that basically made it nearly impossible for our poor and underserved patients to participate. They’re already financially burdened and they’re being asked to pay taxi rides and hotels… they have to do overnight visits often.” The cost of transportation is an important challenge for underserved patients. One report from the Atlantic found that transportation expenses can sometimes equal up to 15% “of what a typical local low-cost household makes in a year.” This is because, even in cities that offer mass transit options, cars remain the most reliable mode of transportation. This is arguably the case in the city of Boston, which remains one of the most congested cities in the United States. Participating in a clinical trial requires frequent trips to and from clinical facilities, at very specific times. This regimen can be especially challenging for cancer patients, who may be too fatigued or impaired to drive themselves. Without the means to arrange for taxis or ride-sharing services, they may be left with few to no options. According to the Lazarex Cancer Foundation “an estimated 95 percent of cancer patients don’t enroll” in clinical trials due to travel concerns.
Given the urgent need to provide more options to persons with cancer and their families, a group of concerned clinical researchers and stakeholders embarked on a five-year journey to pass legislation that would clarify the rules for reimbursing out-of-pocket expenses incurred when participating in a clinical trial. As Dr. Moy explains: “a lot of the study sponsors were unwilling to pay [clinical trial] expenses because they were afraid that it would be considered undue inducement for patients to participate in trials.” Without this type of legislation in place, funders may be accused of influencing people to benefit one cancer center over the other. The bill cleared both the House and Senate last year, and was included in a comprehensive bill that was signed by Massachusetts Governor Charlie Baker on January 2nd, 2021. Thanks to this piece of legislation, reimbursement of travel or other costs related to participating in a clinical trial will no longer be considered an inappropriate incentive to participate. Governmental entities, study sponsors, public and private foundations, corporations, and individuals can now offer financial support and advance health equity in clinical trials. Further, the law extends reimbursements to caregivers and chaperones, an essential component of patient-centered cancer care.
Similar legislations are currently under review in Florida and New Mexico, and have already been passed in California, Pennsylvania, Texas, Illinois and Wisconsin. “I think it’s a really fantastic thing and it helps… It really was a win-win for our patients and frankly for our legislators to show that there’s sensitivity to this issue,” remarked Dr. Moy. The passing of these legislations all over the country shows that both legislators and oncology leaders recognize the importance of diversity in clinical trials, and are willing to lend their support. The expansion of these legislations has the potential to equalize the accessibility of clinical trials for all cancer patients, including those who are underserved, and ensure that all patients are given the opportunity to receive innovative care.
 Beverly Moy, MD, MPH
Beverly Moy, MD, MPH
Clinical Director of the Breast Oncology Program
Director of Community Outreach
Medical oncologist
Massachusetts General Hospital Cancer Center
Dr. Beverly Moy is the Clinical Director of the Breast Oncology Program, Director of Community Outreach, and a medical oncologist at the Massachusetts General Hospital Cancer Center. She is an Associate Professor of Medicine at Harvard Medical School. She received her undergraduate education at the Johns Hopkins University and her medical degree at the Albert Einstein College of Medicine. She received a Master’s degree in Public Health at the Harvard School of Public Health.
Dr. Moy’s specific research interests include breast cancer clinical trials and racial and ethnic disparities in cancer care. She has co-authored more than 100 articles in peer-reviewed journals. She is an investigator on multiple research grants examining cancer care equity, including those funded by the Kraft and Trefler Foundations, Merck Foundation, and the National Cancer Institute. She served as the Chair of the American Society of Clinical Oncology’s Ethics Committee and the Health Disparities Committee. She has served as a chair and panelist for multiple breast cancers. She is the Community Outreach Section Editor for the Oncologist and past editorial board member of the National Cancer Institute’s Adult Treatment Patient Data Query. Dr. Moy also serves on the Board of Directors of the Lazarex Cancer Foundation.
