Alliance program sites are working with regional and community partners to develop and implement comprehensive patient-centered interventions and quality improvement programs in the United States. Following our stated goal of disseminating key findings and lessons learned to promote best practices in patient-centered cancer care, we have included here a collection of peer-reviewed publications and other dissemination opportunities.
For more information, make sure to head over to the resources page, which contains links to other publications and a collection of our video explainers and webinar recordings.
RECENT PUBLICATIONS
August, 2023:
A Descriptive Study of Policy and System-Level Interventions to Address Cancer Survivorship Issues across Six United States Health Systems
Journal of Cancer Survivorship.
Click here to read and download
April, 2023:
Reaching Populations to Address Disparities in Cancer Care Delivery: Results From a Six-Site Initiative. Journal of the National Comprehensive Cancer Network.
Click here to read and download
December 2022:
A learning health system approach to cancer survivorship care among LGBTQ+ communities. Journal of Clinical Oncology – Oncology Practice.
December 2022:
Improving cancer care for underserved populations in an academic and community practice setting: protocol for a community health worker pilot navigation programme. Published in BMJ Open.
May 2022:
Implementing patient navigation programs: Considerations and lessons learned from the Alliance to Advance Patient-Centered Cancer Care. Published in Cancer.
Are you looking for a specific site?
You can skip to your preferred section by clicking on the links below:
- The Georgia Cancer Center for Excellence at Grady Health System
- The Johns Hopkins University School of Medicine
- Massachusetts General Hospital (MGH) Cancer Center
- Northwestern University Feinberg School of Medicine
- The Ohio State University Comprehensive Cancer Center
- The University of Arizona Cancer Center
Improving Cancer Care for Underserved Populations – Considerations to Inform Health Policy
The Alliance National Program Office (NPO)
The University of Michigan School of Nursing serves as the National Program Office (NPO) for the Alliance. The NPO supports program efforts and encourages collaboration among program partners and community-based organizations to share best practices and lessons learned.
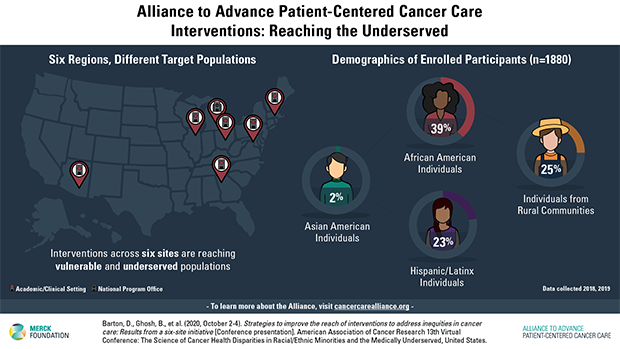
Strategies to improve the reach of interventions to address inequities in cancer care: Results from a six-site initiative
13th AACR Conference on the Science of Cancer Health Disparities in Racial/Ethnic Minorities and the Medically Underserved, Barton D, Ghosh B, Hamann H, Percac-Lima S, Dobs A, Naughton M, Matthews R, Gabram-Mendola S, Simon M, Bueno Y, Moy B, Paskett E, Danner S, Chen B, Ploutz-Snyder R, Friese C, October 2020.
NPO Co-Director Debra L. Barton, RN, PhD, FAAN presented a poster examining the reach of Alliance interventions by comparing the demographics of the population potentially eligible for interventions with those of enrolled participants. The results show that sites are enrolling vulnerable and underserved patient population groups that largely reflect the demographic distribution of the total eligible population.
Registered conference attendees can review this content any time: https://www.pathlms.com/aacr/courses/22851
The Georgia Cancer Center for Excellence at Grady Health System
The GCCE at Grady Health System presented promising results from their interventions at several academic conferences. Included here is a brief overview of their presentations:
The Impact of a Registered Dietitian in an Urban Safety Net Oncology Clinic
Food and Nutrition Conference of the Academy of Nutrition and Dietetics, Forbus MP, Matthews R, Mishra P, Facdol J, Bascho-George V, Coples S, Garrett R, Wang Z, Gabram-Mendola S., October 2020.
A summary of their findings: In a safety net hospital, a registered dietitian intervention significantly changed patients’ viewpoints on the importance of adequate nutrition during cancer treatment. By having an RD/CSO as part of the cancer team, patients also showed a significant change in making conscious healthy choices at mealtimes.
Improving Timeliness of Care for Breast, GYN, and Aerodigestive Cancer Patients with Nurse Navigators in a Safety Net Hospital.
ASCO Quality Care Symposium, C. Rehr, T. Carter, E. Flenaugh MD, Wang Z, G. Ohaegbulam MD, R. Matthews MD, P. Mishra, J. Facdol, S. Coples RN, D. Thomas RN, R. Garrett RN, S. Gabram MD, October 9-10, 2020
A summary of their findings: After the addition of nurse navigators within the cancer program, data showed a decrease in time patients spent between diagnosis and treatment. The intervention focused on breast, GYN, and aerodigestive cancer patients. These measurable improvements over three cancer sites, largely attributed to nurse navigation, suggest that cancer outcomes for patients treated in the safety net hospital will improve over time.
Read more about the Health Systems and Policy changes undertaken by Grady Health System
The Johns Hopkins University School of Medicine
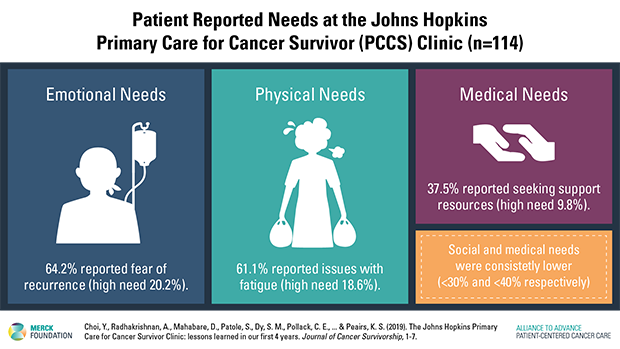
The Johns Hopkins Primary Care for Cancer Survivor Clinic: lessons learned in our first 4 years
Johns Hopkins Medicine established the Primary Care for Cancer Survivor (PCCS) Clinic in 2015 to address the unique needs of survivors of cancer. Between 2015 and 2019, the clinic saw over 230 patients; nearly half were breast cancer survivors. The team learned several valuable lessons along the way. The first one was the importance of building a strong network of referrals, greatly aided by consistent communication with cancer teams. The second was choosing to have survivorship care embedded in general medicine, where patients are viewed as whole individuals, and can receive help for all of their physical and emotional concerns. Lastly, the success of the clinic is attributed to getting crucial buy-in from oncologists and general medicine practitioners alike.
Learn more here: https://doi.org/10.1007/s11764-019-00816-3
Read more about the Health Systems and Policy Change efforts undertaken by Johns Hopkins
Massachusetts General Hospital (MGH) Cancer Center
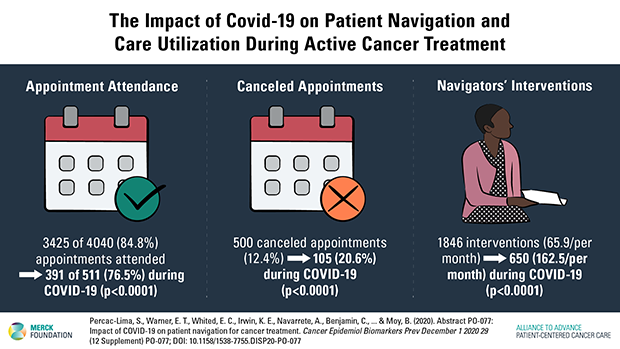
Impact of COVID-19 on patient navigation for cancer treatment
Patient navigation has been shown to improve cancer care in underserved populations. Since November 2017, the Massachusetts General Hospital Cancer Center has been enrolling newly diagnosed cancer patients from three community health centers into a patient navigation intervention. Most of the patients receive primary care in Chelsea, a city that had the highest rate of COVID-19 infection in Massachusetts. Data analysis showed that, although navigators could not provide in-person navigation during COVID- 19, they performed substantially more interventions per month. Patient navigation may be a promising strategy to ensure cancer care for underserved patients during public health crises such as COVID-19.
Learn more here: https://doi.org/10.1158/1538-7755.DISP20-PO-077
Read more about the Health Systems and Policy Change efforts undertaken by MGH
Northwestern University Feinberg School of Medicine
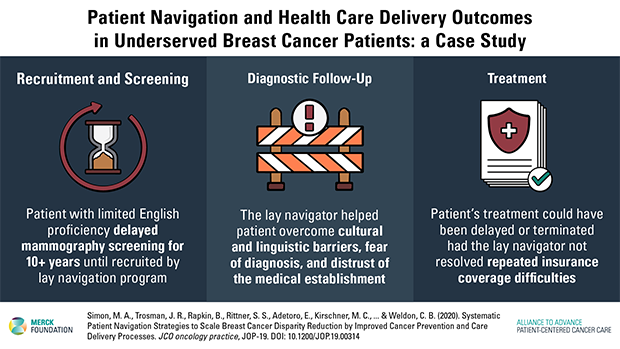
Systematic patient navigation strategies to scale breast cancer disparity reduction by improved cancer prevention and care delivery processes
Northwestern University Feinberg School of Medicine developed the 4R (the Right information and Right care for the Right patient at the Right time) model to provide patients with a clear project plan of their treatment, regardless of how many facilities may be involved in their care or their stage of treatment. Care sequence templates, like the 4R care model, can help a clinical care team to optimize a patient’s care. Data collected from one patient can in turn inform process improvement of patient care and expansion of navigation services at a health system level. A learning health care system approach that systematically integrates data patterns emerging from multiple patient navigation experiences may improve processes of care and reduce cancer disparities.
Learn more here: https://doi.org/10.1200/JOP.19.00314
Read more about the Health Systems and Policy Change efforts undertaken by Northwestern
The Ohio State University Comprehensive Cancer Center
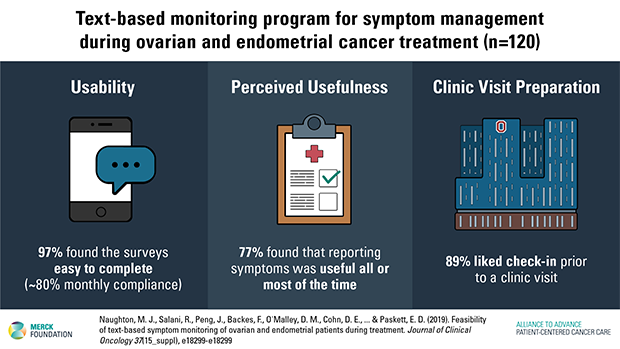
Feasibility of text-based symptom monitoring of ovarian and endometrial patients during treatment
Unreported symptoms during cancer treatment can lead to poorer patient care and quality of life. Newer technology enables effective means to track patients’ health in real time. This quality improvement program evaluated the feasibility of implementing systematic patient symptom monitoring during the first 12 months after a diagnosis of cancer. Patients are asked to respond to a questionnaire once a month, reporting on a variety of psychological and physical symptoms. Survey results are reviewed by specially-trained triage coordinators who, in turn, refer the patient to their physician or to specialized navigation services, if needed.
Learn more here: https://doi.org/10.1200/JCO.2019.37.15_suppl.e18299
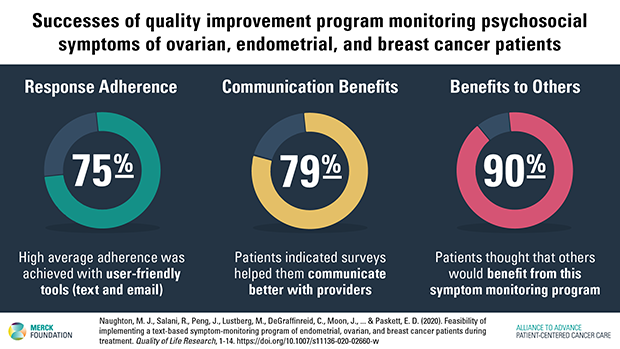
Feasibility of implementing a text-based symptom-monitoring program of endometrial, ovarian, and breast cancer patients during treatment
Patients utilizing this voluntary program had an overall mean age of 60.5 (range 26–87), and 85% were non-Hispanic white. iPhones were provided to 42 patients, and navigation services were used by 69 patients. Average adherence with monthly surveys for all patients was 75%, with breast patients having lower adherence after 5 months. The most commonly reported symptoms across cancer types were moderate levels (scores of 4–7) of fatigue and sleep disturbance. At 6 months, 71-77% of all patients believed the surveys were useful to them and their health care team.
Learn more here: https://doi.org/10.1007/s11136-020-02660-w
Read more about the Health Systems and Policy Change efforts undertaken by the Ohio State University
The University of Arizona Cancer Center
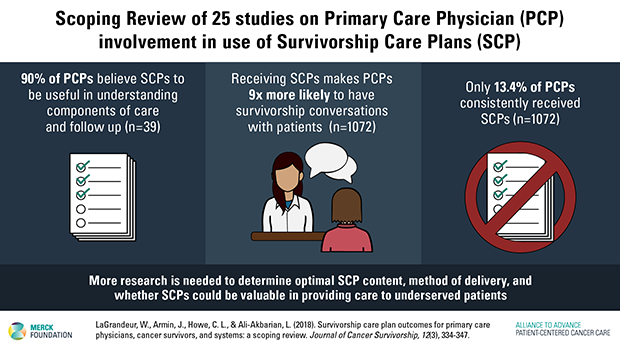
Survivorship care plan outcomes for primary care physicians, cancer survivors, and systems: a scoping review
This paper reviews 25 studies that look at the involvement of primary care physicians (PCPs) in the use of survivorship care plans (SCPs). Survivorship care plans include important guidelines for monitoring and maintaining a person’s health, and are specially tailored to an individual’s health history, diagnosis of cancer, and subsequent treatment. This paper found that although 90% of PCPs believe that SCPs are useful in understanding components of care and follow-up, only 13% consistently received them.
Learn more here: https://doi.org/10.1007/s11764-017-0673-5
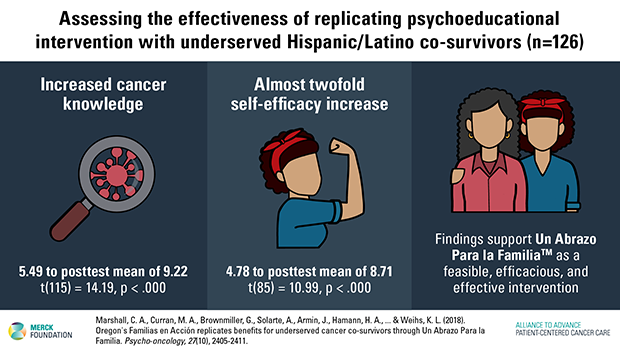
Oregon’s Familias en Acción replicates benefits for underserved cancer co-survivors through Un Abrazo Para la Familia
The paper assesses the effectiveness of reproducing the intervention Un Abrazo Para La Familia™, moving the program from Southern Arizona to Portland, Oregon. Abrazo is a brief (three one-hour sessions), low-cost intervention presented in the language of choice (Spanish or English) of participants. It focuses on understanding cancer as a life-threatening chronic illness by providing specific information on the disease, coping with the diagnosis, and connecting participants with other supportive programs in Arizona. Findings show that participants have an increased understanding of their or their loved one’s diagnosis, and an almost twofold self-efficacy increase. Self-efficacy measures how well an individual can execute a course of action required to deal with a given situation, in this case a diagnosis of cancer. Successfully replicating the intervention in a different environment is a crucial step in assessing its effectiveness.
Learn more here: https://doi.org/10.1002/pon.4841
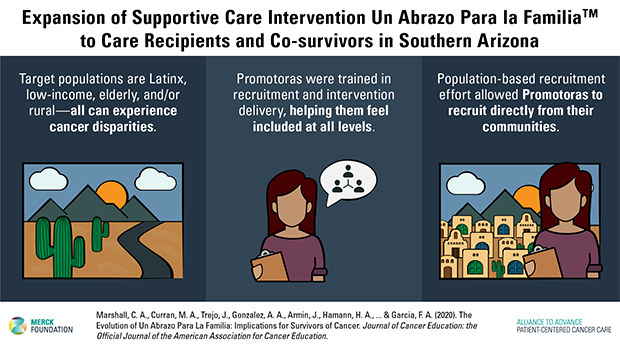
The evolution of Un Abrazo Para La Familia™: implications for survivors of cancer
The team from the intervention Un Abrazo Para La Familia™ shared valuable lessons learned to improve promotora (community health worker) training and increase the project’s effectiveness and efficiency. A competency-based test was delivered in June 2018 to 10 promotoras who had completed the training to examine their ability to successfully deliver the Abrazo intervention. Results show that the trained promotoras demonstrated the necessary skills to lead and direct the Abrazo intervention.
Learn more here: https://doi.org/10.1007/s13187-020-01737-x
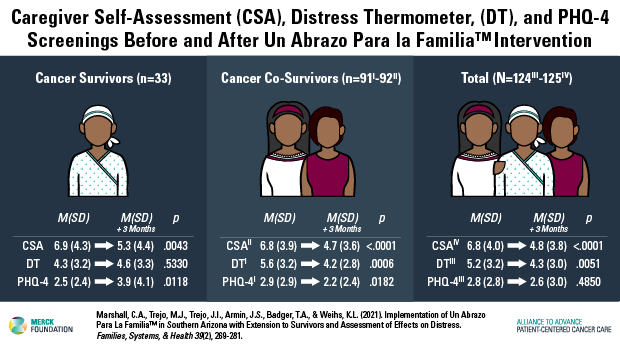
Implementation of Un Abrazo Para La Familia™ in Southern Arizona With Extension to Survivors and Assessment of Effects on Distress
Dr. Catherine Marshall’s latest publication makes the case for adding interventions like Un Abrazo Para La Familia™ to the standard of care. Data show it may improve access to mental health care and help support vulnerable and underserved populations.
Learn more here: https://doi.org/10.1037/fsh0000617
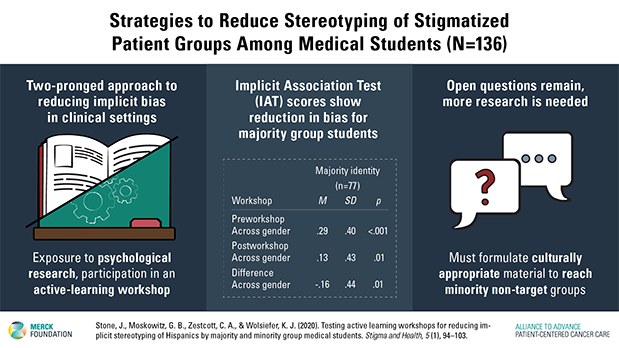
Testing active learning workshops for reducing implicit stereotyping of Hispanics by majority and minority group medical students
This paper analyzes the development of an intervention aimed at reducing the stereotyping of Hispanic patients as medically non-compliant. Controlling the expression of implicit bias in a clinical setting is a very complex balancing act. Physicians need to rely on categorizations based on age, gender, race, and ethnicity when formulating a diagnosis. However, once these biases are activated, physicians need to then “individuate” the patient, developing personalized treatment recommendations and engaging in patient-centered dialogue that will help the patient be fully involved in all treatment decisions.
Learn more here: https://doi.org/10.1007/s00520-020-05468-z
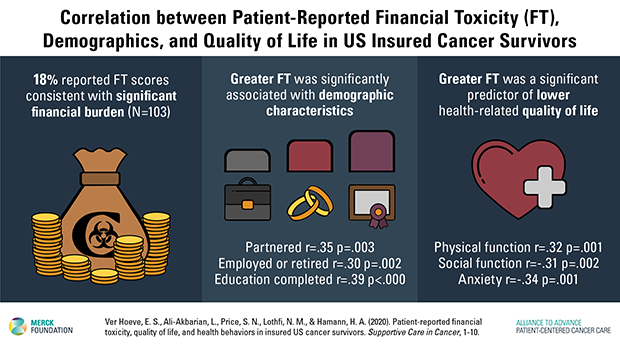
Patient-reported financial toxicity, quality of life, and health behaviors in insured US cancer survivors
The paper examines the concept of financial toxicity (FT) in insured cancer patients. The National Cancer Institute defines financial toxicity as any problem a cancer patient may experience as related to the cost of medical care. Findings show that 18% of patients surveyed reported significant financial burden, with greater FT significantly associated with some demographic characteristics, such as marital status, educational attainment, and employment status. Greater FT was a significant predictor of lower health-related quality of life.
Learn more here: https://doi.org/10.1007/s00520-020-05468-z
Read more about the Health Systems and Policy Change efforts undertaken by the University of Arizona