The Substance Abuse and Mental Health Services Administration has recently released data showing that mental illness is a growing, largely unaddressed public health concern. Their findings show that over 44 million adults have mental illness, and of those, 16 million people (including 3.1 million youths aged 12-17) have experienced a major depressive episode.
In this context, oncology and primary care practitioners are striving to attend to their patients’ mental and physical health, monitoring them for signs of mental distress. Although it is common for 20-30% of patients to experience clinically relevant levels of depression or anxiety when receiving a diagnosis of cancer, according to Dr. Kelly Edwards Irwin of the Massachusetts General Hospital Cancer Center, physicians and patients should not ignore prolonged symptoms of depression. “Depression can be treated effectively with psychotherapy and medication,” she explains. She adds that it is important to address these symptoms because they impact the patient’s quality of life and ability to engage in needed cancer treatment.
Dr. Irwin has spent much of her career working at the intersection of mental health and cancer care, treating vulnerable patients living with a serious mental illness (SMI), defined as a mental health disorder that significantly impacts functioning, such as a psychotic disorder (schizophrenia, schizoaffective disorder), bipolar disorder, and severe major depressive disorder. She reports that even though great strides have been made in the field of patient-centered cancer care, gaps in medical care for disadvantaged populations persist. Her work is part of a larger effort undertaken by the Alliance to Advance Patient-Centered Cancer Care (the Alliance), with multiple sites across the country working on overcoming communication barriers, implicit bias, and any other obstacle that could preclude underserved patients from receiving the information and the treatment they need.
According to Dr. Irwin, caring for patients with SMI means working to overcome profound stigma and significant barriers to care. Her approach utilizes a “flexible and persistent” multi-disciplinary team, developing person-centered solutions that could be adopted as a national model of patient-centered cancer care for many populations experiencing inequities, as she explained: “person-centered care begins with the individual and what they value- not just who they are as a patient”.
As the Substance Abuse and Mental Health Services Administration reports, one in 25 Americans live with a serious mental illness (SMI). Data shows that adults with schizophrenia are dying 25 years earlier than the general population, and cancer is the second leading cause of death. Individuals with serious mental illness experience a 30% higher fatality rate, in part because they are less likely to receive timely, quality cancer care.
According to Dr. Irwin, patients with mental illness may experience multi-layered obstacles that can make it challenging to access adequate medical care. First, patients may have uncontrolled psychiatric symptoms (including fear, depression, and disorganization), lack financial resources or have less social support. The second layer is made up of clinician-related factors, including limited training across disciplines, barriers to communication, and diagnostic overshadowing, or the tendency to attribute medical symptoms to a patient’s mental health condition. A third impediment is structural, related to the health care system as a whole: the separation between mental health and primary and cancer care, no shared access to medical records, and limited access and funding for mental health care.
Preventative care measures and improved care coordination could go a long way towards affecting the health outcomes of cancer patients with SMI, but there are limited resources available to tackle this growing epidemic. Dr. Irwin’s response is the Collaborative Care and Community Engagement Program, an initiative designed to prevent premature cancer mortality and improve the quality of life of individuals affected by mental illness and cancer through clinical innovation, research, education, and advocacy. She has worked with patients who have faced similar barriers to care, and in working with them, she honors the memory of patients who did not have access to the program prior to its inception.
One of the experiences that inspires her work every day is that of Charlie (not his real name), a patient suffering from schizophrenia who passed away from complications related to lung cancer.
Dr. Irwin recounts that Charlie was hospitalized in a state psychiatric hospital because of his persistent disorganization and paranoia that was often directed towards the staff assisting him. During the course of his treatment, he developed a persistent cough, and tests revealed a small mass in his lungs. At that time, the cancer had not progressed beyond early stages, and there were treatment options available. Doctors explained these options to Charlie, but he remained convinced that he could not have cancer. Because of his paranoia, he told doctors that they had somehow given him cancer and declined additional treatment. The doctors noted that he declined cancer treatment and he was not referred for oncology consultation.
Dr. Irwin has seen this dynamic at play often when treating patients with SMI; much like any other cancer patient, they are overwhelmed by the diagnosis of cancer, but in addition, their serious psychiatric symptoms influence their ability to fully comprehend the implications and medical risks. Physicians should be aware that, even though patients may decline medical care, they first need to be informed and fully understand the risks and benefits of their decisions, as Dr. Irwin stresses: “we need to ensure that all patients have access to the information they need to support decision-making. We need to persist.” Many clinicians may lack training in how to negotiate these challenging situations particularly when patients have complex needs and have transitions in care.
One year later, Charlie was discharged to a group home. His discharge plan addressed many challenges including psychosis and substance use but did not prioritize follow-up on the abnormal scan or address the risk of untreated cancer. As his disease progressed, a community mental health nurse noticed Charlie’s increased coughing and weight loss and reached out to Dr. Irwin who advocated for him to be brought to the hospital for a mandated evaluation. Dr. Irwin and the interdisciplinary team took time to explain his diagnosis in more accessible terms and show the images of the scans. Once he was able to understand what he was facing, Charlie agreed to stay in the hospital to be treated.
Dr. Irwin has found that this approach works in an overwhelming majority of cases, as long as a physician takes time to develop a rapport with the patient and the people they trust: “It’s essential to meet people where they are – literally and psychologically, to understand what they value and what care means to them”. Charlie had finally agreed to treatment, but at this point, it had been a full year and a half since his initial diagnosis. Unfortunately, the cancer was no longer curable. Dr. Irwin and the team arranged for Charlie to receive palliative care in his group home where he passed away.
According to Dr. Irwin, Charlie’s story shows the importance of person-centered care and working as a team to build understanding and increase access to care. When working with patients with SMI, clinicians need to question their own assumptions around mental health, and what declining care means, and design solutions that decrease burden for patients, as Dr. Irwin explains: “access to good care shouldn’t be based on luck; it should be developed as a standard of care”. Since Charlie’s passing, Dr. Irwin has established an innovative clinical and research program that addresses disparities throughout the continuum of cancer care, beginning with screening and referrals from oncology and community mental health.
The Alliance to Advance Patient-Centered Cancer Care supports Dr Irwin’s collaboration with the North Suffolk Mental Health Association to proactively identify patients at the time of cancer diagnosis. Once they receive a referral, Dr. Irwin and her team have developed several out-of-the-box solutions to deliver rapid access to specialty care, including same day radiology care for patients who have missed appointments, joint home visits with psychiatry and oncology specialists, and home visits to promote continuity of care from inpatient to outpatient settings. Dr. Irwin is also leading the first randomized trial of a collaborative care model of mental health and cancer care for patients with SMI at cancer diagnosis.
In addition, Dr. Irwin has been very active with advocacy and education, developing Bridging the Divide: Cancer and Mental Health, an annual symposium that brings together 250+ clinicians, researchers, advocates, policy-makers, patients and caregivers to build awareness and generate solutions that can inform health care guidelines and policy. In addition to advocating for patients with SMI as a population experiencing inequities that lead to premature mortality, Dr. Irwin emphasizes the importance of expanding the dialogue around mental health and cancer to all patients: “We need to invest in mental health care at the time of cancer diagnosis for all people affected by mental illness”. Her hope is that her work with the Alliance will generate the evidence necessary to disseminate her intervention on a national level.
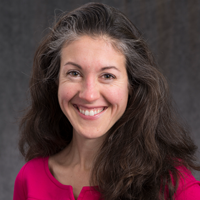 Dr. Kelly Irwin
Dr. Kelly Irwin
Dr. Kelly Irwin is an Assistant Professor of Psychiatry at Harvard Medical School and a faculty psychiatrist at the Massachusetts General Hospital (MGH) Cancer Center and MGH Schizophrenia Program. She is the founding director of the Collaborative Care and Community Engagement Program, a clinical and research program dedicated to improving cancer outcomes for individuals with serious mental illness at the Mass General Cancer Center. Dr. Irwin also collaborates with the Department of Mental Health to increase access to cancer care for individuals with serious mental illness in the community. Dr. Irwin graduated from Harvard University in 2001, Harvard Medical School in 2008, and the Harvard Chan School of Public Health in 2017.
Dr. Irwin investigates why people with severe mental illness including schizophrenia and bipolar disorder are more likely to die from cancer and develops interventions to improve cancer outcomes throughout the continuum of cancer care. Dr. Irwin conducted a successful pilot of an interdisciplinary intervention incorporating proactive psychiatry consultation and case management at cancer diagnosis for patients with serious mental illness and is now leading a follow-up randomized trial funded by the National Cancer Institute. Her research has been funded by the American Cancer Society, the Patient-Centered Outcomes Research Institute, Harvard Medical School, and the Massachusetts Department of Mental Health and featured in an editorial in the New England Journal of Medicine. In recognition of her innovation in clinical care, research, and advocacy, she was named one of the One Hundred leaders who are changing the face of cancer care delivery.
