The article published on the JCO Oncology Practice offers a novel approach to incorporating patient navigation services into larger health systems. Dr. Melissa Simon of the Northwestern University Feinberg School of Medicine and her team describe their process of utilizing data derived from their breast cancer patient navigation program to systematically improve care delivery for the vulnerable populations they aim to serve.
Simon, M. A., Trosman, J. R., Rapkin, B., Rittner, S. S., Adetoro, E., Kirschner, M. C., … & Weldon, C. B. (2020). Systematic Patient Navigation Strategies to Scale Breast Cancer Disparity Reduction by Improved Cancer Prevention and Care Delivery Processes. JCO oncology practice, JOP-19. https://ascopubs.org/doi/abs/10.1200/JOP.19.00314
The recent article published in JCO Oncology Practice by Alliance to Advance Patient-Centered Cancer Care program partner Dr. Melissa Simon of the Northwestern University Feinberg School of Medicine offers a novel approach to incorporating patient navigation services into larger health systems. In the article, Dr. Simon and her team describe their process of utilizing data derived from their breast cancer patient navigation program to systematically improve care delivery for the vulnerable populations they aim to serve. While the positive impact of patient navigation programs is known, it has not been effectively advanced beyond a one-on-one approach between navigator and patient. Thus, this newly published study is the first “to propose systematically incorporating the data/insights gained from patient navigators into cancer care delivery processes through a learning health care system approach that uses 4R care sequence templates.” The 4R intervention, also known as the Right information and Right care for the Right patient at the Right time, provides patients with a clear project plan of their treatment. The care plan should enable patients to access supportive care services regardless of the location of care, income, race/ethnicity, or other factors.
The article highlights the experience of one patient—who was served through Northwestern’s grant-funded breast cancer patient navigation program—tracing her experience through screening, diagnosis, multiple surgeries, and insurance troubles. She received the help of a lay patient navigator every step of the way. The navigator was able to help assuage the patient’s mistrust and help her reengage with the medical system at multiple critical junction points to receive the care she needed. Via a detailed, step-by-step analysis of the patient’s navigation, the study team demonstrates the positive value that patient navigation brings to the patient experience while making a strong case for more robust, system-wide, data-driven integration.
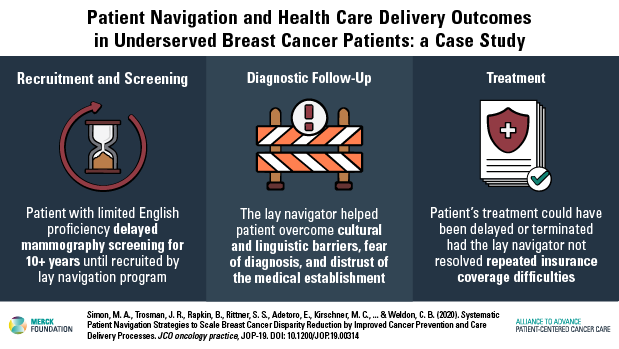
This case study methodologically assesses “common barriers to the access of medically underserved women” that have been pre-identified and categorized through the Patient Navigation Research Program (PNRP)—an NCI developed program to establish and evaluate a generalizable patient navigation program for vulnerable patient populations (Freund et al., 2008).
Importantly, the Northwestern team uses this approach to identify “suboptimal areas of care coordination” within their own health system and navigation process that would be improved through more systematic patient navigator integration. The team sheds light on specific aspects of care coordination that, in this case, could have been improved: genetic counseling, dental care, flu vaccination, family planning, and other possible chronic disease management. This feedback is an integral part of the iterative process of their data-driven approach. By incorporating patient navigator feedback from patient experiences into the health system’s 4R sequence templates, the Northwestern team would be able to start to offer a broader and increasingly more effective patient navigation program.
At the policy level, whereas many patient navigator programs are funded through soft-money or individual grant awards, Dr. Simon and her team aim to prove the utility of system-wide adoption of patient navigation and the importance of embedding permanent and sustainable patient navigation programs within hospitals and community health clinics. By advancing patient navigation through recommendations grounded in experiential data— implementing a learning healthcare system approach wherein process improvements increase the value of patient navigation —Dr. Simon’s study demonstrates how to scale patient navigation programs to successfully benefit and reduce care disparities in underserved and vulnerable patient populations.
References:
Freund K.M., Battaglia T.A., Calhoun E., et al (2008). National Cancer Institute Patient Navigation Research Program: Methods, protocol, and measures. Cancer 113 (pp. 3391-3399)
